CBT and DBT are both counselling approaches. What do they mean and what is the difference?
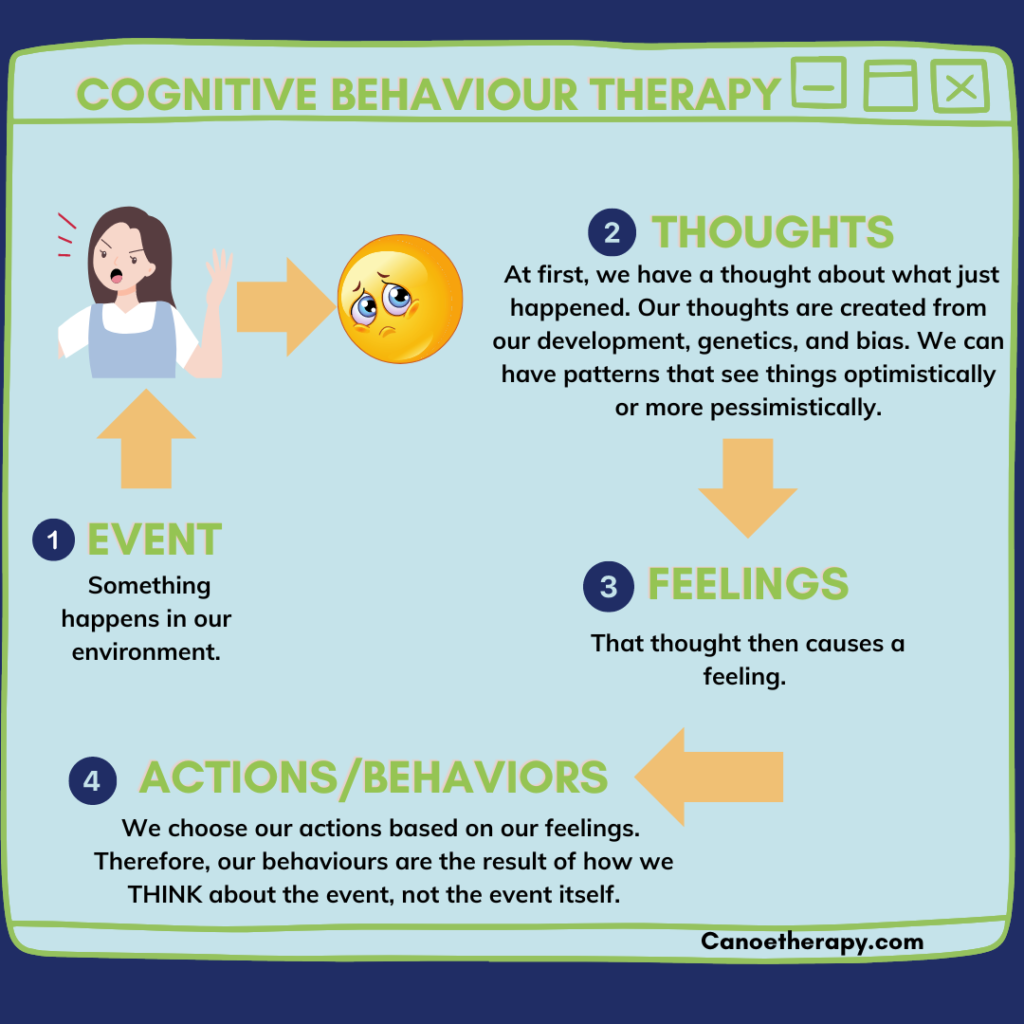
CBT stands for Cognitive Behaviour Therapy. At its core, CBT refers to the premise that all feelings and actions are preceded by a thought. When a person has a negative pattern of thought, that will create either lower moods, or anxious thoughts. The feelings then cause the person to act in manner that can cause the low mood to persist. In simple terms, change the thoughts, change the mood which will change the actions. CBT helps clients uncover what automatic thoughts they have and help them to be in greater control of their thoughts, shifting them to more realistic or positive thoughts, thereby helping to bring about more positive moods and actions. CBT is very evidence based and is found to be a powerful tool for helping improve mood disorders and reducing anxiety.
DBT was originally developed to help clients with more severe mood disorders, but is now used as an effective tool in mainstream counselling sessions. Dialectical means “the existence of opposites.” In DBT, people are first thought to accept that they are having big or difficult feelings; they learn to accept the presence of big feelings and at the same time, learn that not all feelings are an indication of danger or trouble. Acceptance is a cornerstone of DBT. Once the client masters acceptance, they begin to learn strategies for managing those feelings; one of the biggest strategies is being able to be aware of some feelings but to learn they do not need to act on every feeling. Accepting, understanding and managing moods and feelings is central to DBT and the process includes a lot of strategies to help equip clients to achieve contentment.
Our therapists are CBT and DBT informed and use strategies that fit each unique client. The process of counselling tends to be more of an art than a science and there is no prescribed approach. We have big tool boxes of theories, strategies, styles and will adjust to help make the most of each session with each client.
Cognitive-Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are both therapeutic approaches that fall under the broader category of cognitive-behavioral therapies. They share some similarities but also have distinct features.
Cognitive-Behavioral Therapy (CBT):
Meaning:
CBT is a widely used and evidence-based form of psychotherapy that focuses on the connection between thoughts, feelings, and behaviors. It is based on the premise that our thoughts influence our emotions and behaviors, and by identifying and changing negative thought patterns, individuals can experience improvements in their emotional well-being.
Key Components:
- Cognitive Restructuring: Involves identifying and challenging irrational or negative thought patterns and replacing them with more balanced and realistic ones.
- Behavioral Activation: Focuses on increasing engagement in positive and healthy behaviors while reducing avoidance and withdrawal.
- Homework Assignments: Clients often engage in activities or exercises between sessions to practice and reinforce the skills learned in therapy.
- Goal-Oriented: CBT is typically goal-oriented and often a short-term, structured therapy.
Applications:
CBT has been successfully applied to a wide range of mental health issues, including anxiety disorders, depression, phobias, and more.
Dialectical Behavior Therapy (DBT):
Meaning:
DBT is a specific form of cognitive-behavioral therapy developed by Dr. Marsha Linehan. It was initially designed to treat individuals with borderline personality disorder (BPD) but has since been adapted for various conditions characterized by emotional dysregulation.
Key Components:
- Mindfulness: DBT places a strong emphasis on mindfulness, helping individuals become more aware of their thoughts, feelings, and behaviors in the present moment.
- Distress Tolerance: Teaches skills to cope with distressing situations without resorting to destructive behaviors.
- Emotion Regulation: Focuses on understanding and managing intense emotions effectively.
- Interpersonal Effectiveness: Provides tools for improving communication, navigating relationships, and asserting one’s needs.
Applications:
DBT is often used for individuals with borderline personality disorder, but it has also proven effective for those dealing with self-destructive behaviors, mood disorders, and other conditions involving emotional dysregulation.
Key Differences:
- Emphasis on Mindfulness:
- CBT may incorporate mindfulness, but it is a central component of DBT.
- DBT places a strong emphasis on being present in the moment, observing thoughts and feelings without judgment.
- Target Population:
- CBT is widely applicable to various mental health conditions.
- DBT was initially developed for borderline personality disorder but has been adapted for other conditions involving emotional dysregulation.
- Therapeutic Style:
- CBT is often more structured and directive.
- DBT may involve a more collaborative and acceptance-based approach.
- Use of Validation:
- DBT places a significant focus on validation as a way to acknowledge and accept a person’s experiences without necessarily agreeing with their behaviors.
Both CBT and DBT can be highly effective, and the choice between them may depend on the specific needs and characteristics of the individual seeking therapy. In some cases, therapists may integrate elements of both approaches to tailor treatment to the client’s unique situation.